The article 'Biosimilars in nephrology' focuses on the introduction and use of biosimilars in the field of nephrology, highlighting the importance of these biological medicines similar to the originals for the treatment of kidney diseases and renal anemia. The content of the article is summarized below:
The article begins by noting that pharmaceutical companies have increased their research and production of biological medicines due to their high specificity and effectiveness in the treatment of various diseases. These medicines represent approximately 30% of the global pharmaceutical market and have contributed significantly to the care of patients with chronic and serious diseases.
Biosimilars are introduced, which are biological medicines similar to the original biological products (reference products). Biosimilars have proven to be equivalent in efficacy, safety and quality to original biologicals, and offer economic advantages that help maintain the sustainability of health systems.
It is mentioned that, in the field of nephrology, there were initially concerns about the safety of erythropoietin biosimilars due to rare cases of pure red cell aplasia in patients receiving parent erythropoietin. These problems were related to the immunogenicity of the products and the variability in their production.
The article details the fundamental differences between biological medicines and chemically synthesized medicines, highlighting that the former are high molecular weight macromolecules, while the latter are small, well-defined molecules. Furthermore, biologic drugs may be immunogenic due to their subtle structural differences and the presence of impurities.
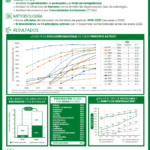
The process of development and authorization of biosimilars by the European Medicines Agency (EMA) is discussed, which includes quality studies, preclinical studies and comparative clinical studies to demonstrate biosimilarity with the reference product. The importance of evaluating the immunogenicity of biosimilars is also emphasized.
The article highlights that the interchangeability of biosimilars with reference products depends on national decisions, and it is mentioned that some European countries have supported the interchangeability of these medicines due to their high similarity.
In nephrology, biosimilars have mainly been used in erythropoiesis-stimulating agents (ESAs) to treat renal anemia. A list of ESA biosimilars authorized by the EMA is provided. Phase 1 and clinical studies are mentioned that demonstrate the therapeutic equivalence and safety of these biosimilars compared to reference products.
The article also refers to biosimilars of rituximab, eculizumab and basiliximab, highlighting their use in the treatment of various conditions, although there is no mention of specific biosimilars approved by the EMA for these medicines at the time of writing the article.
In summary, the article highlights the importance of biosimilars in the field of nephrology and provides information on their development, licensing and use in the treatment of kidney diseases and renal anemia. The need for comprehensive studies to demonstrate the biosimilarity and safety of these drugs compared to reference products is emphasized.