Biosimilar medicines, like generic medicines, offer the same guarantees of quality, safety and efficacy as the original products and are guaranteed and accredited by the European Medicines Agency (EMA) and approved by the European Commission. In no case, however, can biosimilars be interpreted as “the generic version” of biological medicines. There are major differences between the two medicines (biosimilars and generics) in terms of their nature, manufacturing process, development cost, legal route and approval regulations, and also in how they are used by healthcare professionals.
Generic medicines have their origin in chemical structures and are considered identical to their reference medicines. Biosimilars, on the other hand, are drugs of biotechnological origin that are much more difficult to manufacture. Its development is very similar to that of reference biological medicines. In fact, the general principles of drug development and review by European authorities apply to biosimilar medicines to the same extent as to reference biologics.
A great economic effort
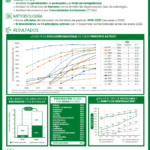
Putting a biosimilar medicine on the market also involves a much greater economic effort than for generics. Investments ranging between 75 and 250 million euros are required, and clinical trials for seven years or more.
Another important difference -which should not be ignored- is that biosimilar medicines are not prescribed by active principle and substitution between the biosimilar drug and its reference medicine is not possible by the pharmacist.
"A biosimilar and a generic are not comparable concepts, their correct use requires a specific legislative environment"
These are the main reasons why the approval of a specific regulation for biosimilar medicines is necessary. A regulation in which, following the trail set by the European Union, it is established that only the doctor can exchange a biotechnological drug for a biosimilar; and where the concepts of "interchangeability" and "substitution" are clarified.
Likewise, it is essential to develop an information and training plan that implements a correct knowledge of biosimilar medicines that helps both doctors and patients to understand the scientific support that protects and guarantees them, and that puts an end to false myths. and speculations that circulate around these drugs, especially among certain market players. It is the health administration that must assume this function and convey to health professionals and patients confidence in the use and consumption of these drugs.
In this new legal framework, supply policies and conditions must also be defined. The Autonomous Communities, with the support of the Ministry of Health, must promote systems to encourage the prescription and use of biosimilars as an essential measure to encourage cost containment and access to biological treatments for more patients.
In addition, a proprietary system for pricing and reimbursement should be established. The removal of biosimilar medicines from the Reference Price System (SPR) is urgent. The SPR was created to allow substitution between drugs included in the same set, something that cannot be applied to biosimilar drugs. The law determines that these medications are not substitutable. Consequently, they should not become part of homogeneous sets to determine their price.
A biosimilar medicine cannot be considered a generic and, therefore, it is essential not to treat it as such at any level: therapeutic, economic or, in any case, regulatory. Its future as a sustainable and quality option in the treatment of various serious and debilitating diseases depends on it.
Angel Luis Rodriguez de la Cuerda
CEO of BioSim