The article titled 'The Impact of Policy Interventions to Promote the Adoption of Biosimilar Medicines in Belgium: An Interrupted Time Series Analysis at the National Level' discusses the efforts made by the Belgian government to promote the use of biosimilar medicines and evaluates their effectiveness.
Biosimilars are similar versions of authorized biological medicines, which offer cost-effective alternatives while maintaining safety and efficacy standards. These medications have the potential to reduce healthcare costs and improve patient access to treatments. The European Medicines Agency has established a solid regulatory framework for biosimilars, guaranteeing their quality and safety.
Belgium, like many other countries, faces the challenge of rising healthcare costs, with biological medicines contributing significantly to pharmaceutical budgets. The article emphasizes the need for a competitive and sustainable off-patent biological medicines market in Belgium to control expenses. Despite this need, Belgium has struggled to achieve high biosimilar adoption rates compared to other European nations.
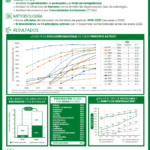
The study investigates the impact of various policy interventions implemented by the Belgian government to promote the use of biosimilars. It employs interrupted time series analysis, using data from the Belgian National Institute for Health and Disability Insurance (NIHDI). The analysis focuses on three specific biosimilar molecules: etanercept (in outpatient care), filgrastim, and epoetin (both in hospital settings).
In the ambulatory care sector, the study evaluates the impact of a financial incentive for prescribers implemented in 2019. Results indicate a significant reduction in etanercept biosimilar prescriptions following this intervention.
In the hospital environment, two policy interventions are analyzed. The first intervention, implemented in 2016, includes prescribing targets for biosimilars and monitoring hospitals for appropriate bidding. This led to a modest decline in quarterly adoption of epoetin biosimilars. The second intervention involved a biosimilar information campaign, resulting in a notable increase in quarterly adoption of epoetin biosimilars and an immediate increase in the use of filgrastim biosimilars.
However, the study suggests that the impact of these policy interventions has been variable and limited. The need for a more comprehensive policy framework to establish a competitive and sustainable off-patent biological medicines market in Belgium is highlighted.
In conclusion, the article highlights the challenges Belgium faces in promoting the adoption of biosimilars and the importance of effective policy interventions. While some measures have shown positive effects, the overall impact has been inconsistent. The study emphasizes the need for a comprehensive approach to address the barriers to the adoption of biosimilars in the Belgian healthcare system and ensure their long-term sustainability.